Oncology Practice Management and the Practice Management Institute are proud to present our exclusive series on optimizing the patient experience. In next month’s edition, we present strategies to address scheduling challenges. This article was reviewed by Jan Hailey, MHL, CMC, CMCO, CMIS, CMOM, CMCA-E/M.
Working in an oncology practice requires not only medical expertise but also a high degree of emotional intelligence, especially when it comes to interacting with patients who are understandably experiencing a range of intense emotions. Encounters with angry patients are not uncommon; however, these situations must be approached with effective strategies to ensure both the patient’s well-being and the maintenance of a safe and supportive practice environment. Drawing on recommendations from leading health organizations and best practices, this article aims to provide oncology office staff with useful guidance on how to communicate with angry patients.
Anger in patients may stem from various sources, including fear, frustration, grief, dissatisfaction, and the feeling of a lack of control over one’s health situation. The American Psychological Association emphasizes the importance of understanding the underlying causes of anger.1 Whether the patient is expressing anger about waiting, billing, or medical issues, there are several factors members of the staff must keep in mind to de-escalate the encounter:
- Recognize that oncology patients are often under significant stress
- Do not take the confrontation personally
- Maintain a professional attitude
- Use effective communication techniques
Communication Techniques
Practice Active Listening
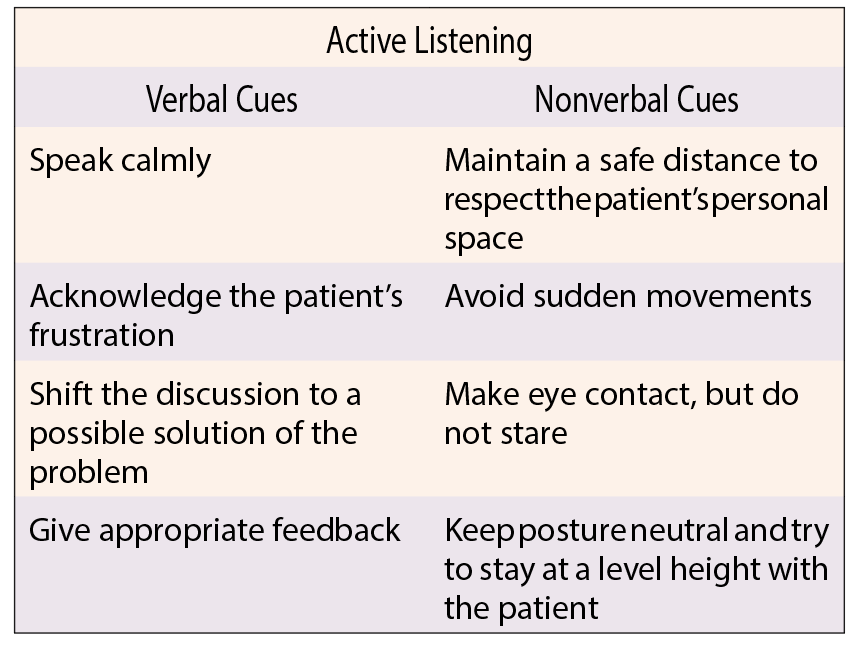
Active listening is crucial. Recommended active-listening techniques include listening without interrupting, acknowledging the patient’s feelings, and showing empathy through verbal and nonverbal cues.2
Maintain Calmness
The Mayo Clinic advises staff to remain calm and to speak in a low, steady voice, as mirroring the patient’s anger can escalate the situation.3
Use De-escalation Techniques
De-escalation techniques, such as those outlined by the Crisis Prevention Institute, include allowing the patient space, not taking the anger personally, and using supportive language.4
Set Boundaries
An American Medical Association (AMA) post dealing with patients’ bad behavior highlights the importance of setting boundaries respectfully if a patient’s anger turns into aggression, ensuring the safety of both staff and the patient. As an example, the AMA post quotes Amy Nicole Cowan, MD, as concluding, “My message to whomever I am correcting is always the same, ‘I care about you as a person, but I will not tolerate offensive behavior. Now let’s focus on how I can help you today.’”5
Provide Information
Providing clear and concise information can empower patients and alleviate the feeling of helplessness that is often the basis of patient anger. The Institute for Healthcare Communication stresses the role of clear communication in patient care and notes that the ability to “explain, listen, and empathize” can profoundly affect patients.6 Imparting information appropriately may not only improve a patient’s current attitude in the office but may also help the patient to follow medical recommendations and thus have beneficial long-term effects on the patient’s overall health.6
Best Practices for Resolution
Problem-solving Approach
As recommended by the Oncology Nursing Society (ONS), adopting a problem-solving approach can help address the specific concerns of the patient.7 The problem-solving approach has many variations, but standard techniques include defining the problem, considering possible solutions, evaluating and choosing an option, and implementing and following up on the chosen solution. An angry patient needs to feel listened to, so it is important to offer empathy to allow patients to maintain trust in the staff for problem-solving to occur.
Follow-up Measures
The ONS also suggests follow-up with patients who have experienced outbursts to address any unresolved issues and to reassure them of the practice’s commitment to their care.7
Staff Training
Regular training sessions for staff on communication and de-escalation techniques are vital to maintain effective communication skills. The National Cancer Institute has published a detailed summary on communication in cancer care and recommends training for clinicians and support staff.8
Conclusion
Effective communication with angry patients is a skill that can be developed and refined. By employing empathy, active listening, and de-escalation techniques, and by providing clear information and support, office staff can navigate these challenging interactions and contribute to a therapeutic and supportive oncology practice environment.
References
- American Psychological Association. Understanding anger: how psychologists help with anger problems. Accessed January 23, 2024. www.apa.org/topics/anger/understanding
- Chipidza F, Wallwork RS, Adams TN, Stern TA. Evaluation and treatment of the angry patient. Accessed January 25, 2024. www.ncbi.nlm.nih.gov/pmc/articles/PMC5035812/
- Mayo Clinic. Anger management: 10 tips to tame your temper. Accessed January 23, 2024. www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/anger-management/art-20045434
- Crisis Prevention Institute. De-escalation tips. Accessed January 23, 2024. www.crisisprevention.com/Blog/De-escalation-Tips
- American Medical Association. The do’s and don’ts of calling out a patient’s bad behavior. Accessed January 25, 2024. www.ama-assn.org/delivering-care/ethics/do-s-and-donts-calling-out-patients-bad-behavior
- Institute for Healthcare Communication. Impact of communication in healthcare. Accessed January 23, 2024. https://healthcarecomm.org/about-us/impact-of-communication-in-healthcare/
- Traeger L, Park ER, Sporn N, et al. Development and evaluation of targeted psychological skills training for oncology nurses in managing stressful patient and family encounters. Oncol Nurs Forum. Accessed January 25, 2024. www.ons.org/pubs/article/232766/download
- National Cancer Institute. Communication in Cancer Care (PDQ)–Health Professional Version. Accessed January 25, 2024. www.cancer.gov/about-cancer/coping/adjusting-to-cancer/communication-hp-pdq
Interested in measuring your patients’ experience?
About the Reviewer

Jan Hailey is a WPS Government Health Administrators (Medicare) Provider Outreach and Advisory Group member and has been instrumental in developing Practice Management Institute’s Workforce Initiatives program. She has a Master of Health Leadership degree and five professional certifications in office management, coding, insurance processing, auditing, and compliance.


