The November 2016 presidential elections have cast a shadow in many minds about the future of the transition from the volume-driven, fee-for-service healthcare delivery model to the value-based care model. With the current promises of repealing and replacing the Affordable Care Act (ACA) of 2010, physicians and healthcare providers are left guessing as to what they will be expected to do, and where their future is heading.
It also remains to be seen what will happen to the Center for Medicare & Medicaid Innovation (CMMI) and the Oncology Care Model (OCM). If the new administration decides to repeal and replace the ACA as a whole, the alternative payment model path may be in jeopardy. However, the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) is likely to stay, given that it was one of the most agreed-upon pieces of legislation during the previous administration and was passed with bipartisan support—392-37 in the House and 92-8 in the Senate.1
An important foundation of the ACA was the establishment of CMMI, which is charged with establishing pilot programs for alternative payment models across multiple specialties. CMMI defined and approved the concept of bundled payment structures, including the OCM and the Comprehensive Care for Joint Replacement model.
Post-ACA legislation, passed with bipartisan support in 2015, repealed the Medicare sustainable growth rate and replaced it with MACRA.1 The institution of MACRA paved the way for transitioning providers who were not enrolled in an Alternative Payment Model pilot to the value-based care model, now called the Quality Payment Program.2,3
The Oncology Care Model
CMMI announced the first phase of the Alternative Payment Model of the OCM to align provider incentives with quality and cost-savings and improve the patient’s experience. The OCM was launched on July 1, 2016, as the most physician-focused Alternative Payment Model to date. Overall, 196 practices (representing 3200 oncologists) were selected to participate, and 16 national and regional payers are planning to implement the OCM in 2017.
Administering chemotherapy to designated diagnoses in the OCM triggers an OCM episode. Unlike the traditional fee-for-service model, OCM providers are expected to take greater consideration for the patient’s cost of care with a 6-month bundle payment, supplemented by a monthly care coordination payment of $160 to enhance care transformation.
OCM providers must offer standard-of-care treatments based on nationally recognized guidelines, and report quality metrics using CMMI-recommended parameters to enable gain-sharing after a discount, as determined by the Centers for Medicare & Medicaid Services (CMS).
The primary goal of reforming the payment system is to encourage and reward providers who are willing to accept the imminent paradigm shift in healthcare delivery. Financial incentives are aligned to improve care and outcomes for patients with cancer who receive chemotherapy.
Practices participating in the OCM pilot are required to perform the following 6 transformation processes:
- Provide patient navigation
- Document a 13-point care plan in accordance with Institute of Medicine recommendations
- Provide 24/7 access to a qualified clinician, with real-time access to patients’ medical records
- Use treatment in accordance with recognized treatment guidelines
- Monitor data to improve quality
- Use electronic health records that are certified by the Office of the National Coordinator for Health Information Technology.
The OCM pilot program is in its third quarter of implementation. Although the majority of OCM practices are still learning the ropes of reporting requirements, the OCM pilot is at full throttle. It remains to be seen how many practices will opt for the 2-sided risk model when the time comes.
The Quality Payment Program
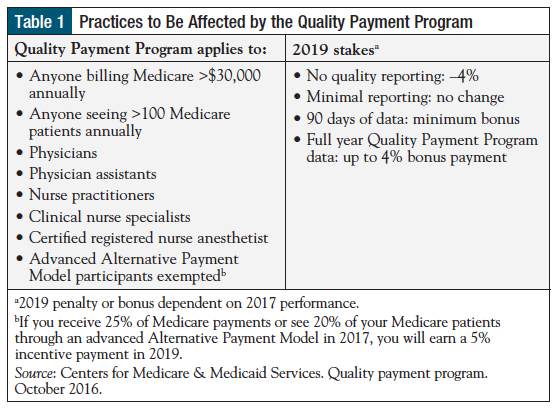
Compared with the OCM, the majority (>80%) of practices will fall in the Quality Payment Program under MACRA.4 There is significant confusion about what those practices will need to change, and what they will report. Those who are willing to transform and transition successfully to value-based care will be eligible to receive significant bonuses, beginning in 2019. Originally defined as the Merit-based Incentive Payment System (MIPS), the Quality Payment Program will affect Medicare reimbursement for the majority of providers (Table 1).
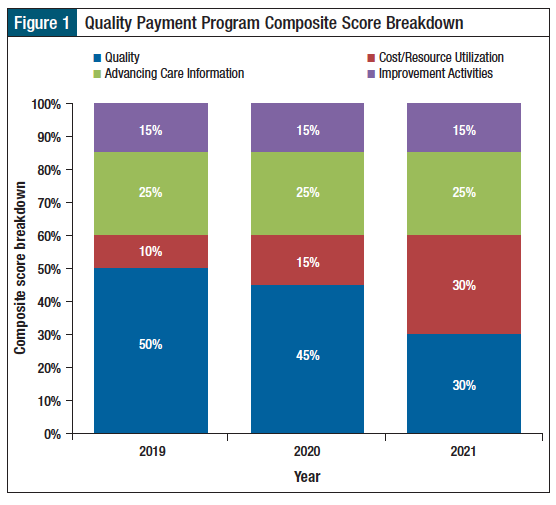
The Quality Payment Program defined elements of performance measures in practice transformation under 4 categories, including Quality Performance, Cost/Resource Utilization, Improvement Activities, and Advancing Care Information.2,3
Quality Performance
This measure replaces the Physician Quality Reporting System. Providers will be assessed based on their performance of quality measures that are included in the final MIPS quality measures list and on their performance of quality measures that are specified in qualified clinical data registries.
CMS published 19 general oncology measures, which are based on effective and efficient clinical care, patient safety, patient experience, and population health.4 Eligible providers or groups will be required to report at least 6 quality measures, including 1 outcome measure, for 50% or more of their patients. If fewer than 6 measures apply to a provider or group, the provider or group must report on all applicable measures.
If there is no applicable outcome measure, the provider or group must report a high-priority measure instead.
Cost/Resource Utilization
Physicians and groups will be scored in the resource utilization category in a similar manner to the quality performance category. CMS will assign 1 to 10 points to each measure based on the provider’s performance against a benchmark for the specified performance period. The cost/utilization performance category will be weighted at 0% in 2017.
Improvement Activities
Physicians and groups are expected to show improved health outcomes under the Improvement Activities category. This measure will be assigned a score based on a 40-point scale. A maximum performance score of 40 will be assigned to clinicians and groups that are certified as patient-centered medical homes. MACRA also required that practices participating in the Alternative Payment Model receive 50% of the maximum score (20 points) in this performance category.5
Advancing Care Information
This category replaced the earlier program known as Meaningful Use. The MACRA rule reinstates a 90-day reporting period for 2017 and 2018, allowing—for the first time—group reporting of electronic health record use.5 Advancing Care Information creates a new scoring mechanism to assess electronic health record use. All Advancing Care Information measures are based on modified stage 2 or 3 Meaningful Use measures.
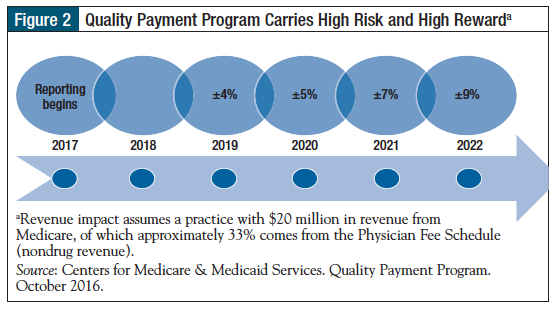
What does this all mean in pure financial terms? At Carolina Blood and Cancer Care Associates, we have prepared a predictive model based on the average revenue of a 5-physician group oncology practice, and the numbers are astounding, in terms of rewards and penalties (Figure 1).
The Oncology Care Model versus the Quality Payment Program
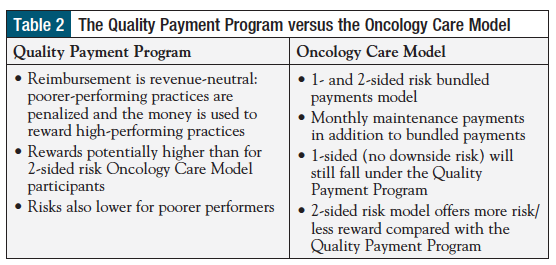
The OCM is in its infancy, whereas the Quality Payment Program is a newborn (Table 2). An intriguing challenge for the majority of early adopters of the OCM is: do we stay with the OCM and move on with 2-sided risk, or do we stay with the 1-sided risk and prepare to move toward the Quality Payment Program? An objective analysis of the risks versus rewards (Figure 2), in our opinion leans toward MIPS, based on the Quality Payment Program track.
The OCM’s long-term pathway expects practices to improve annually versus their own baseline performance, whereas the Quality Payment Program compares the practice’s performance with that of its peers.
The majority of practices that chose to participate in the OCM are clearly forward-thinking, and some of them have already established processes that led to higher efficiency, better patient experience, and lower cost in advance of the OCM. It would be extremely difficult for these practices to keep improving their performance. In fact, such practices may be penalized for being early adopters.
Furthermore, a downside risk in the OCM could reach up to 20% of their gross payment for spending more than their target benchmark. Such a drastic level of penalty for situations that are sometimes beyond a practice’s control exposes the practice to risk for continued survival under the wrong circumstances.
However, under the Quality Payment Program track, early adopters who have transformed their processes to be more efficient, improved their clinical process, and adopted the required technology standards, are more likely to have significant bonuses (ie, up to 27% for the small number of exceptional performers) against a negative overspending risk of 3% (ie, the financial resource utilization component of the Quality Payment Program path).
References
- Medicare Access and CHIP Reauthorization Act of 2015, Pub L No. 114-10, 129 Stat 87.
- Centers for Medicare & Medicaid Services. Quality payment program. October 2016. https://qpp.cms.gov/. Accessed March 7, 2017.
- Centers for Medicare & Medicaid Services. Quality Payment Program. Executive Summary. October 14, 2016. https://qpp.cms.gov/docs/QPP_Executive_Summary_of_Final_Rule.pdf.
- Centers for Medicare & Medicaid Services. Quality Payment Program. Quality measures. https://qpp.cms.gov/measures/quality#. Accessed March 7, 2017.
- Centers for Medicare & Medicaid Services. Medicare program; merit-based incentive payment system (MIPS) and alternative payment model (APM) incentive under the physician fee schedule, and criteria for physician-focused payment models. Final rule with comment period. Fed Regist. 2016;81:77008-831.